Arm Lift is also known as Brachioplasty
It is a surgical procedure that:
1. Reduces excess sagging skin that droops downward
2. Tightens and smoothes the underlying supportive tissue that defines the shape of the upper arm
3. Reduces localized pockets of fat in the upper arm region
In short, the upper arm is tightened with the removal of excess skin.
Why does the skin on the arms sag?
It can be due to various reasons, including:
– weight fluctuations
– ageing
– genetics
Who is a good candidate?
– those who present with very bad upper arm skin laxity
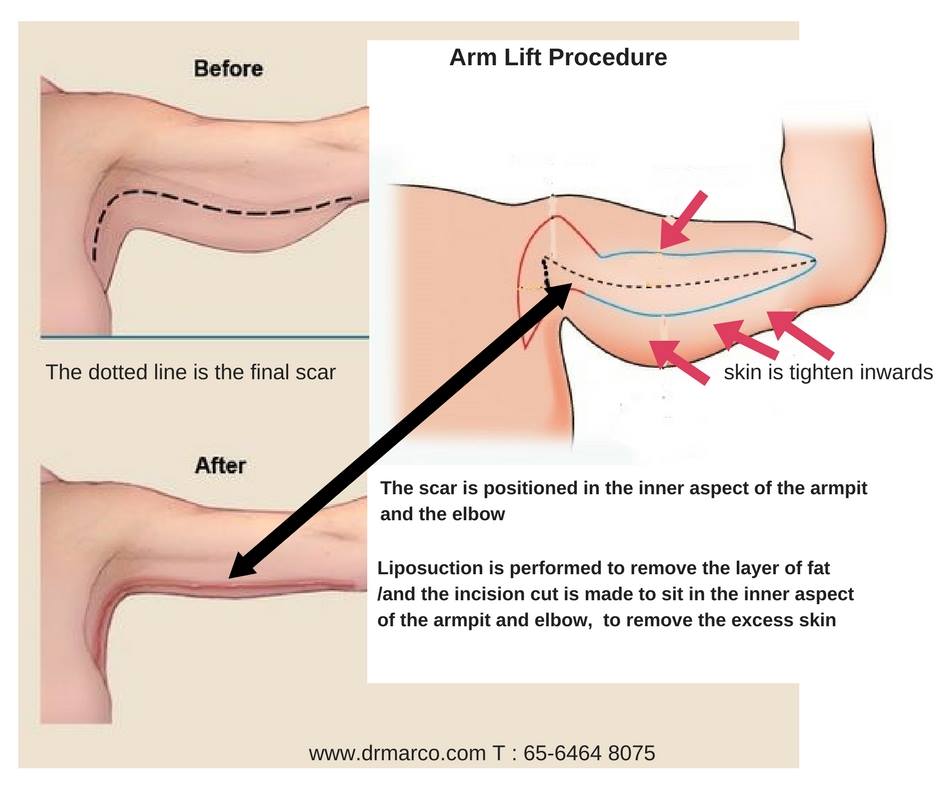
According to Dr Marco, the location of the incision depends on a few factors, such as:
– Arm flabbiness
– Skin elasticity
– Amount of excess skin
– Amount of fat for removal
– Amount of skin to remove and tighten
Dr Marco said incision placement can be done in the following locations:
– inner arm
– back of the arm
– within the folds at the armpit
Based on years of experience, Dr Marco prefers doing an inner arm incision since they tend to heal better and the scar is not so visible.
Dr Marco said the main goals are to tighten the arm and to hide the scar along the natural creases/folds in the armpit as well as the inner arm. Based on our body anatomy of our arm muscles, there is a natural line between our biceps and triceps muscles. The trick in plastic surgery is using the anatomical line to dissimulate the scar.
This technique gives a long-lasting result. With this incision, it’s possible to remove a lot of the excess skin and tighten them, while lifting the skin around the elbow area.
After the surgery, patients must maintain their weight and also continue to exercise their arms to maintain strong muscle tone in the arms. For the scar, it will depend on the individual own healing.
To know more about the above procedure, call our clinic today at 65-6464 8075 to consult Dr Marco.









 What will it affect?
What will it affect?